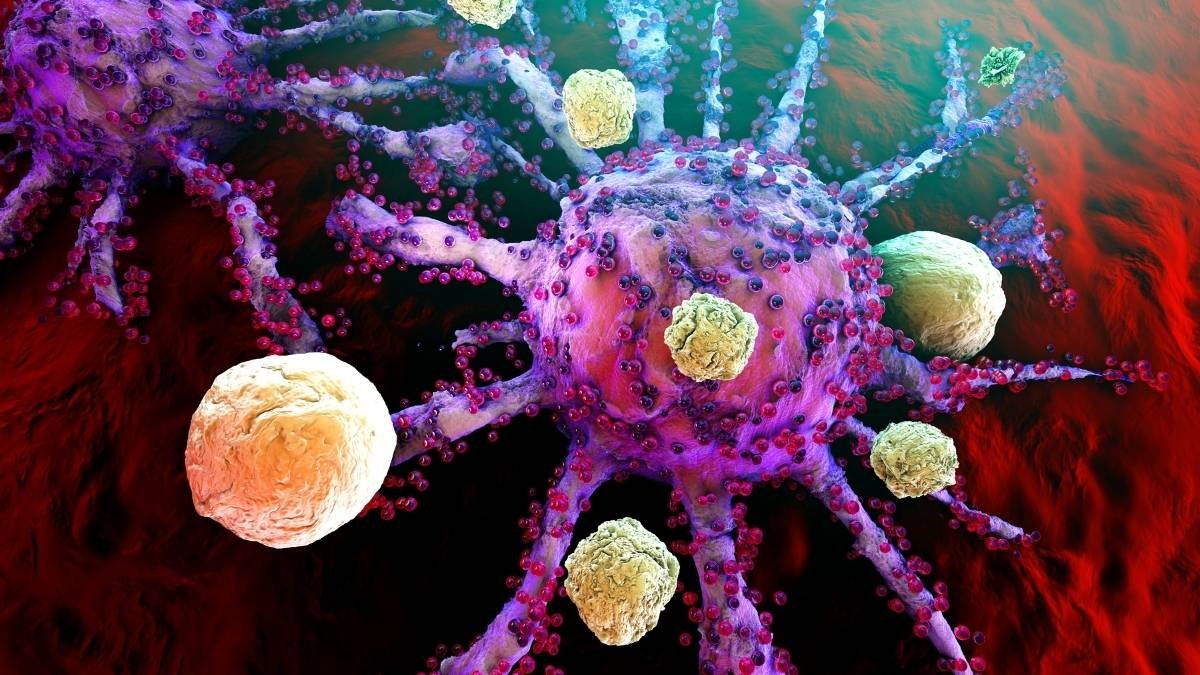
Your immune system is supposed to be your personal bodyguard, but for millions, it has turned into the attacker. Living with an autoimmune disease means fighting a civil war inside your own body, a battle that leaves you exhausted, in pain, and searching for real answers.
The number of people affected is growing fast, and it’s clear that old explanations about bad genes aren’t the full story. New research is pointing to an unexpected culprit and a powerful new ally: your gut.
This isn’t just another health trend. Scientists are now showing exactly how the trillions of tiny bugs living inside you could hold the key to calming the storm and reclaiming your health.
Why Autoimmune Problems Are on the Rise
Why Are So Many People Getting Autoimmune Diseases?
If you have an autoimmune disease, you are not alone. These conditions, where your body’s defense system attacks its own healthy parts, are becoming a major health problem. There are more than 100 different types.
In the United States, millions of people are affected. And it’s not just here. A huge 2023 study in the United Kingdom looked at 22 million people and found that about one in ten now has an autoimmune disorder. It’s more common in women (13%) than in men (7%), which is a known pattern.
What’s really concerning is how fast these numbers are growing. The rate of new cases is going up quickly around the world. Our genes haven’t changed that fast. This tells scientists that something else is going on.
They are now looking closely at our environment—things like our diet, lifestyle, and the chemicals we’re exposed to every day.
It has been hard to track these diseases because there hasn’t been a good system for it. But that’s changing.
Top health groups, like the U.S. National Institutes of Health (NIH), are now making it a priority. They are creating new plans to help researchers work together to figure out why this is happening and how to stop it.
Why Your Gut Might Be the Real Cause
For a long time, doctors thought autoimmune diseases were all about having the wrong genes. But that’s not the whole story. It now seems to be a mix of three main things: your genetic makeup, your environment, and the health of your gut.
Your gut has become the main focus of new research. It’s the primary place where the outside world—food, germs, and more—meets your body’s defense system.
Your gut is more than just a food processor; it’s a command center for your immune system. About 70% of your immune cells live there, ready to check on everything that passes through.
At the same time, your gut is home to trillions of tiny bugs—bacteria, viruses, and fungi—known as the gut microbiome. This community of microbes is so important that some call it our “second genome.” These bugs help you get nutrients from food, manage your metabolism, and even affect your mood.
This new information changes how we think about autoimmune disease. It’s not just your immune system failing. It’s often a sign that the friendly relationship between you and your gut bugs has broken down.
Two main things go wrong: your gut bugs get out of balance (a state called dysbiosis), and the lining of your gut gets damaged (a condition known as “leaky gut”).
When your gut is healthy, your microbiome helps keep your immune system calm and balanced. But when that balance is lost, your gut can become a source of constant irritation.
This puts your immune system on high alert and can set the stage for it to start attacking your own body. The goal for future treatments is not to wage war on the immune system, but to act more like a gardener, restoring the natural balance inside of you.
How Your Body Loses Control (And How to Get It Back)

The idea of a single “master switch” for autoimmune disease is a simple way to think about it, but the reality is more involved. Your immune system has many checks and balances to keep it from attacking you.
Two of the most important parts of this system are the “brakes” inside your cells and the physical wall of your gut lining. When these two things fail, problems can start.
The “Brakes” of Your Immune System: A Nobel Prize-Winning Discovery
Think of your immune system like a car. It needs a gas pedal to attack germs, but it also needs brakes to stop it from crashing into your own body.
A huge step forward in medicine was the discovery of the cells that act as these brakes. In 2025, three scientists—Mary Brunkow, Frederick Ramsdell, and Shimon Sakaguchi—won the Nobel Prize for this work.
They identified a special type of immune cell called a regulatory T-cell, or Treg. The job of Tregs is to patrol your body and stop any rogue immune cells that might attack your healthy tissues. They are the security guards that keep the peace.
The scientists found that a single gene, Foxp3, is the master controller for these Treg cells. When this gene is broken, the result is a severe, body-wide autoimmune disease. This was proof that Tregs are essential.
In many common autoimmune diseases, it seems these Treg “brakes” are not working correctly. This allows inflammation to run wild. As one immunologist put it, “If you control the brakes to the immune system, it gives you the ability to turn the immune response up or to tone it down.”
This discovery has started a whole new area of research. Scientists are now working on treatments to boost these Treg cells to calm down autoimmunity. They are also trying to turn them down to help the immune system fight cancer.
This Nobel Prize was a big deal because it showed that the future of medicine is about making the immune system smarter and more balanced, not just stronger.
Your Gut Lining: The Gatekeeper for Your Health
If Tregs are the immune system’s police force, then your gut lining is its border wall. This wall is made of a single layer of cells that are sealed together with something called “tight junctions.”
These junctions act like gates, carefully controlling what gets absorbed from your gut into your bloodstream.
A key problem in many autoimmune diseases is that this wall breaks down. This is often called “leaky gut.”
When the tight junctions get loose—from things like a bad diet, stress, or infections—the wall is no longer secure. Substances that should stay inside the gut can leak into the rest of your body. This includes undigested food, toxins, and bits of bacteria.
When these things leak into your blood, your immune system sounds a massive alarm. It launches an attack, causing low-grade inflammation that never turns off. Over time, this constant state of alert can confuse the immune system, causing it to start attacking your own body’s tissues.
This changes how we see the problem. The issue is often not “bad” bacteria, but normal bacteria ending up in the wrong place. A bug that is harmless in your gut can become a major problem if it gets into your bloodstream.
This means that healing and sealing the gut wall is one of the most important things you can do to prevent or manage these conditions. It’s better to fix the fence than to chase after every cow that gets out.
What Happens When Your Gut Bugs Are Out of Balance?
The health of your gut wall and the balance of your gut bugs are closely connected. When your gut’s ecosystem is out of whack—a state called dysbiosis—it affects your entire immune system.
Dysbiosis usually means one of three things: you’ve lost too many of your good bugs, the bad bugs have started to take over, or you’ve lost the overall variety of bugs.
Lots of research now shows a clear link between dysbiosis and autoimmune conditions like rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes.
For example, people with lupus often have less variety in their gut bugs and a different ratio of certain bacteria families.
This imbalance causes several problems. First, you produce less of the good chemicals your gut bugs make, especially short-chain fatty acids (SCFAs), which are vital for a healthy gut and a calm immune system.
Second, an overgrowth of certain bugs can directly damage the gut lining, making it leaky. Finally, the wrong mix of bugs can send constant “danger” signals to your immune system, keeping it in a state of inflammation.
Scientists now think of a healthy gut like a healthy rainforest. It’s not about having one specific “perfect” bug.
It’s about having a rich and diverse community of bugs that can work together and bounce back from problems. This idea provides a strong foundation for using diet and lifestyle to create a healthy inner world.
Meet the Troublemakers: Specific Gut Bugs Linked to Autoimmune Disease

While the ideas of a leaky gut and unbalanced bugs are helpful, the strongest proof comes from studies that point to specific bacteria and show exactly how they can cause disease. These studies are the “smoking guns” that show how our own microbes can turn against us.
How One Gut Bug Can Trigger Lupus
A series of important studies led by immunologist Dr. Martin Kriegel gave us a clear example of a gut bug directly causing an autoimmune disease. His team showed how a bug called Enterococcus gallinarum can lead to lupus, a disease that can harm almost any organ in the body.
Here’s how it happens, step by step:
- The Escape. When the gut wall is leaky, E. gallinarum can escape from the intestines and travel to other parts of the body, like the liver and spleen.
- The Alarm. Once it’s outside the gut, the bug triggers a very specific and harmful immune response. It causes the body to make a lot of inflammatory T-cells, which are known to cause tissue damage.
- The Mistake. The bug also causes the immune system to make antibodies that attack the bug’s RNA. But these antibodies make a mistake—they also attack the person’s own human RNA. This kind of self-attack is a classic sign of lupus.
- The Proof in People. The scientists didn’t just see this in mice. They found DNA from E. gallinarum in the livers of people with lupus, but not in healthy people. This suggests the same escape happens in humans.
The most powerful proof came from another experiment. The researchers made a vaccine using a dead version of E. gallinarum.
When they gave this vaccine to mice that were likely to get lupus, it stopped the bug from escaping, halted the self-attacking antibodies, and prevented the deadly disease. A vaccine against other gut bugs did nothing.
This was a huge breakthrough. It showed that a treatment targeting just one specific microbe could stop an autoimmune disease without shutting down the whole immune system.
Other Gut Bacteria That Can Cause Trouble
The case of E. gallinarum is not the only one. More research is finding other specific gut bugs that are involved in different autoimmune conditions.
For example, researchers at the Mayo Clinic found a strong link between a bug called Eggerthella lenta and rheumatoid arthritis (RA). In lab studies, they found that this bug triggers the self-attacking antibodies seen in RA long before any joint pain starts.
This suggests the gut is where the problem begins. The bug seems to work by changing the levels of certain amino acids, making the immune system act much older than it really is. This link was especially strong in female patients, which might help explain why more women get RA.
Another example comes from Harvard Medical School. Researchers there looked at a bug called Morganella morganii and its link to major depressive disorder, which is now seen as having inflammatory and autoimmune parts.
They found something new and alarming. This bug can take a common chemical from the environment (called DEA, found in many products) and build it into one of its own molecules.
This new, altered molecule becomes a powerful trigger for inflammation in the body and brain. This shows a complex link between our genes, our gut bugs, and the chemicals we are exposed to.
These examples, along with others, paint a clear picture. The gut microbiome is not just standing by; it is an active player in autoimmune disease.
| Microbial Species | Associated Condition(s) | How It Causes Trouble |
| Enterococcus gallinarum | Lupus, Autoimmune Hepatitis | Escapes the gut and travels to the liver; turns on inflammatory cells and causes the body to make antibodies that attack itself. |
| Eggerthella lenta | Rheumatoid Arthritis (RA) | Triggers self-attacking antibodies before symptoms appear; makes the immune system act older than it is. |
| Morganella morganii | Depression, Brain Inflammation | Mixes with an environmental chemical to create a molecule that causes strong inflammation. |
| Prevotella copri | Rheumatoid Arthritis (RA) | Believed to be a possible trigger for the inflammation that leads to RA. |
| Ruminococcus gnavus | Lupus, Crohn’s Disease | Linked to disease flare-ups in lupus; makes a sugar molecule that irritates the immune system in Crohn’s. |
The Chemicals Your Gut Bugs Make (And Why They Matter)
Your gut bugs don’t just affect you by being there. They also produce a huge number of chemicals that act as messengers between them and your body. These chemicals can either promote inflammation or help keep the peace.
The most important of these messengers are short-chain fatty acids (SCFAs). You can’t get these from food. They are made only when your good gut bacteria ferment the fiber you eat. These molecules are like a superfood for your gut and immune system.
Here’s what they do:
- They feed your gut wall. One SCFA, called butyrate, is the main fuel for the cells that line your gut. A good supply keeps the gut wall strong and prevents leaks.
- They calm your immune cells. SCFAs help the “brake” cells of your immune system (the Tregs) to grow and work properly, which is key to preventing autoimmune attacks.
- They reduce inflammation. By keeping the gut wall strong and helping the Tregs, SCFAs create a calm, anti-inflammatory environment throughout your body.
When your gut bugs are out of balance, often because of a low-fiber diet, you don’t make enough of these SCFAs. This leads to a weaker gut wall, poorly working immune “brakes,” and a state of inflammation that can lead to many diseases.
This is why a diet full of different plant fibers is so good for you. You’re not just eating “roughage.” You are giving your gut bugs the raw materials they need to make the very chemicals your immune system needs to stay balanced and healthy.
What’s Next? New Ways to Treat Autoimmune Disease

This new knowledge about the gut is leading to a revolution in how we treat autoimmune diseases. We are moving away from treatments that just shut down the immune system and toward smarter therapies that fix the balance that has been lost.
Smarter Treatments Are Coming
Old treatments for autoimmune disease often act like a sledgehammer, shutting down your whole immune system. This can help with symptoms, but it also leaves you at risk of getting sick. The new treatments being developed are much more precise.
Here are some of the exciting new ideas:
Microbiome-Targeted Therapies:
This is more than just taking a generic probiotic. Scientists are working on “next-generation” probiotics with specific strains of bacteria known to help.
They are also exploring Fecal Microbiota Transplantation (FMT), a procedure to completely reset a person’s gut bugs.
Targeted Enzyme Therapies:
This is a very clever approach. For example, researchers at Emory University found an enzyme that can modify the specific bad antibodies that cause myasthenia gravis, a muscle-weakening disease.
The enzyme makes the antibodies harmless without affecting the rest of the immune system. In mice, it was 4,000 times more powerful than current treatments.
“Inverse Vaccines”:
A normal vaccine teaches your immune system to attack a germ. An “inverse vaccine” would do the opposite: it would teach your immune system to tolerate a part of your own body that it’s mistakenly attacking.
This could stop a disease like multiple sclerosis or type 1 diabetes in its tracks without weakening your ability to fight infections.
Pathobiont-Specific Therapies:
Based on the research with lupus, scientists are thinking about creating treatments that go after the specific “bad bugs” that are causing trouble. The vaccine that worked in mice is a perfect example of this.
All of these new approaches share one big idea: repair the system, don’t demolish it. They aim to restore the body’s natural balance. This promises treatments that are not only more effective but also much safer.
Why This Research Is Now a National Priority
This new way of thinking isn’t just happening in labs. It’s now a focus of national policy. In September 2025, the U.S. National Institutes of Health (NIH), one of the world’s top medical research organizations, released its first-ever strategic plan just for autoimmune disease research.
This is a big deal. It means these diseases are now seen as a major public health priority, on the same level as cancer or heart disease.
The five-year plan was created with help from scientists, doctors, and patients. Its goal is to speed up discoveries and get better results for the millions of people who are affected.
The plan focuses on a few key areas:
- Speeding up basic science to understand what causes these diseases.
- Finding better and faster ways to diagnose and treat them.
- Understanding why people often get more than one autoimmune disease.
- Building better tools and systems for research.
- Working closely with patients and communities.
The plan puts a special focus on finding these diseases at their earliest stages, even before symptoms appear, and figuring out how to prevent them.
It’s a roadmap for smarter, more patient-focused research that sees these conditions as connected problems with common roots—many of which lead back to the gut.
An Actionable Guide for 2025: Fortifying Your Gut-Immune Axis

The science is clear: the health of your gut is a powerful tool you can use to manage autoimmune conditions. While amazing new medical treatments are on the horizon, there is a lot you can do right now.
The research gives us a clear guide for diet and lifestyle changes that can help you build a healthy microbiome, a strong gut wall, and a calmer immune system.
Foundational Principles of an Immune-Modulating Diet
Think of your gut like a garden. You want to feed the flowers (the good bugs) and pull out the weeds (the bad bugs). While everyone is a bit different, some basic rules can help almost anyone create a healthier inner garden.
- Maximize Fiber-Rich Foods: This is the most important rule. Fiber from a wide variety of plants is the main food for your good gut bugs. When they eat fiber, they make the anti-inflammatory SCFAs your body needs. Eat lots of vegetables, fruits, whole grains, and beans.
- Incorporate Fermented Foods (Probiotics): Foods like yogurt, kefir, sauerkraut, and kimchi contain live, helpful bacteria. Eating them regularly can add more good bugs to your gut garden.
- Include Prebiotic Foods: Prebiotics are like fertilizer for your good bugs. They are special types of fiber found in foods like garlic, onions, leeks, asparagus, and bananas.
- Focus on Anti-Inflammatory Fats: Healthy fats, especially omega-3s, are great at fighting inflammation. You can find them in fatty fish (like salmon), flaxseeds, chia seeds, and walnuts. Use extra virgin olive oil for cooking.
- Eliminate Inflammatory Triggers: It’s just as important to stop feeding the weeds. Cut back on highly processed foods, which have unhealthy fats and additives. Avoid refined sugar, which feeds bad bacteria. And stay away from industrial seed oils (like soybean and corn oil).
Following these rules can shift your gut from a place of inflammation to a place of peace and balance. Every bite you take is a choice that can either help or hurt your inner ecosystem.
Strategic Dietary Protocols: A Comparative Guide
If you want a more structured plan, a few specific diets are popular for managing autoimmune conditions.
The Autoimmune Protocol (AIP) diet is a very strict elimination diet that can help you find your personal trigger foods. The Mediterranean diet is a more flexible and balanced approach that is easier to follow for a long time.
You should always talk to a doctor or a registered dietitian before starting a new diet. This table can help you understand the differences.
| Feature | Autoimmune Protocol (AIP) Diet | Mediterranean Diet |
| Main Idea | A short-term, strict diet to find your trigger foods and heal your gut. | A long-term, flexible eating style focused on whole foods and healthy fats. |
| What to Eat | Vegetables (but not nightshades), quality meat and fish, fermented foods, healthy fats. | Fruits, vegetables, whole grains, beans, nuts, seeds, fish, and olive oil. |
| What to AVOID | Very Strict: Grains, beans, dairy, eggs, nuts, seeds, nightshade vegetables (like tomatoes and peppers), processed foods, sugar, alcohol, and coffee. | Red meat (in small amounts), processed foods, and sugar. |
| Main Goal | To find out exactly which foods cause your symptoms so you can create a personalized long-term diet. | To reduce your risk of chronic disease and inflammation with a healthy, sustainable way of eating. |
| Who It’s Best For | People with serious symptoms who are very motivated to find their specific food triggers. It’s best to do this with professional help. | People looking for a less restrictive, proven way to improve their health and manage symptoms for the long haul. |
Critical Lifestyle Levers for Immune Resilience
Food is a huge part of gut health, but it’s not the only part. To truly manage an autoimmune condition, you also need to look at other parts of your life that affect your gut and immune system. Your brain and your gut are constantly talking to each other, so your mental state has a real physical effect on your body.
Stress Management:
Chronic stress is terrible for your gut. A “troubled brain will send signals to your gut,” which can mess with your gut bugs and lead to a leaky gut and inflammation.
This can trigger autoimmune flares. Making time for stress relief is not a luxury; it’s a medical need. Try meditation, deep breathing, gentle yoga, or just spending time in nature.
Sleep Optimization:
Your gut and your sleep are deeply connected. Not getting enough good sleep can harm your gut microbiome and increase inflammation. At the same time, a healthy gut helps you sleep better. Aim for 7-9 hours of quality sleep each night.
Create a good routine by going to bed at the same time, turning off screens an hour before bed, and making your room cool, dark, and quiet.
Appropriate Physical Activity:
Regular movement is good for your gut bugs and your immune system. Exercise helps you have a more diverse microbiome. For people with autoimmune conditions, low-impact activities like walking, swimming, or yoga are often best because they don’t put too much stress on the body.
Mindful Medication Use:
Some medicines, while necessary, can be hard on your gut. Antibiotics can wipe out your good bugs, and long-term use of some painkillers (NSAIDs) can damage the gut lining. It’s important to talk to your doctor about the risks and benefits of any medication.
Use them only when you really need to and ask about other options when possible.
These lifestyle habits are not small things. A stressful day or a bad night’s sleep is a real physical event that can make your gut more inflammatory. Managing stress and sleep is a key part of any plan to calm your immune system.
Building Your Team: Partnering with Healthcare Professionals
Trying to manage an autoimmune condition with diet and lifestyle is a big task, and you shouldn’t do it alone. It’s very important to work with healthcare professionals who can guide you.
Always talk to your main doctor or specialist before you make any big changes to your diet or lifestyle. It’s also a good idea to build a team. This might include a gut specialist (a gastroenterologist), a registered dietitian who has experience with autoimmune conditions, or a functional medicine practitioner.
You should also be careful with supplements. While some probiotics might be helpful, the market is not well-regulated, and many products don’t have good science behind them. The wrong probiotic could even make your symptoms worse.
Always get advice from a knowledgeable healthcare provider before you start taking supplements. They can help you choose the right ones for your specific needs. Working together with a team is the safest and most effective way to use these strategies as part of your overall care plan.